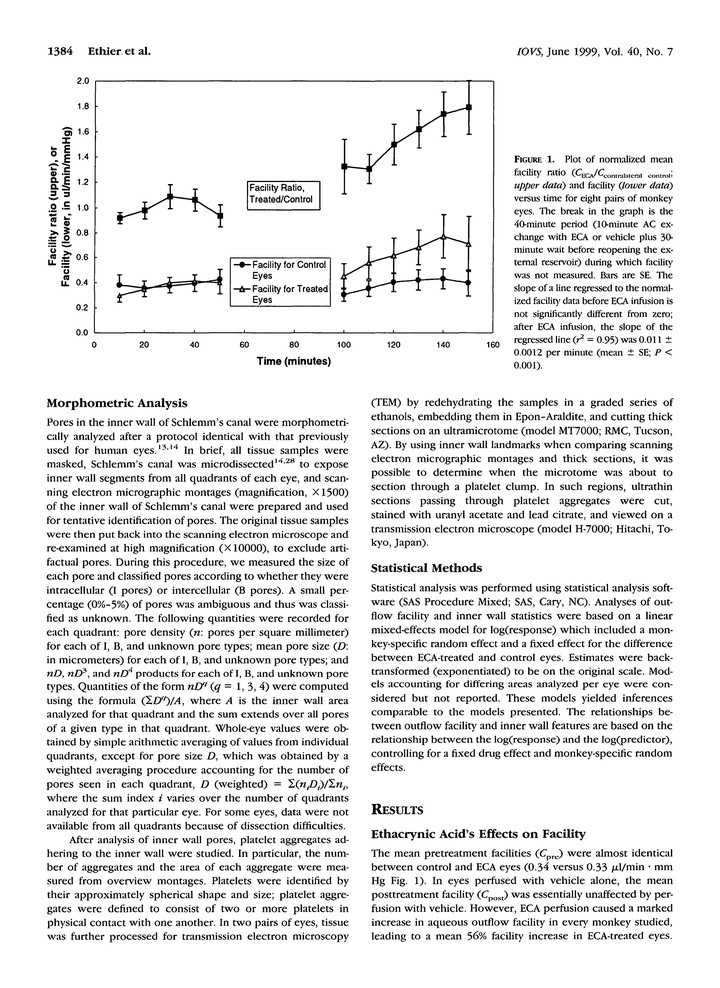
Enthacrynic and acid effects on inner wall pores in living monkeys
Abstract
PURPOSE: The influence of the inner wall of Schlemm’s canal on aqueous outflow facility remains poorly understood. We examined the relationship between inner wall pore characteristics and outflow facility in living primate eyes in which facility had been pharmacologically increased by ethacrynic acid (ECA) infusion and in contralateral control eyes. METHODS: Outflow facility (two-level constant pressure perfusion) was measured in eight pairs of living monkey eyes before and after administration of a bolus dose of either 0.125 mM ECA or vehicle. After exsanguination, eyes were fixed in situ under constant-pressure conditions (mean fixation pressure approximately 19 mm Hg). The density and diameter of inner wall pores and the number and area of platelet aggregates on the inner wall of Schlemm’s canal were measured by scanning electron microscopy. RESULTS: In ECA-treated eyes, outflow facility increased 63% (P < 0.0001), intracellular pore density decreased 46% (P = 0.0094), intracellular pore size increased 27% (P = 0.049), platelet aggregate density increased 158% (P < 0.0001), and area covered by platelets increased 210% (P = 0.012) relative to contralateral controls. Although the average density and size of intercellular pores were essentially unaffected by ECA, an increased density of large (> or = 1.90 microm) intercellular pores was seen in ECA-treated eyes. The density of intracellular pores increased with the duration of fixative perfusion. Other than a weak negative correlation between outflow facility and intracellular pore density in ECA-treated eyes (P = 0.052), facility was not correlated with inner wall pore features. CONCLUSIONS: Our data are most consistent with a scenario in which ECA promotes formation of large intercellular pores in the inner wall of Schlemm’s canal, which are then masked by platelet aggregates. Masking of intercellular pores, combined with fixation-induced alteration of inner wall pore density, greatly complicates attempts to relate facility to inner wall structure and suggests that in vivo pore density is smaller than in fixed tissue. Additionally, facility-influencing effects of ECA on the juxtacanalicular tissue cannot be excluded.