Factors associated with systemic hypertension in asthma
Abstract
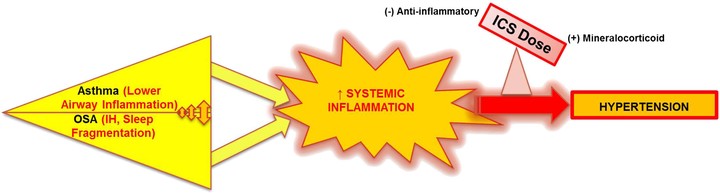
PURPOSE: Asthmatics have unique characteristics that may influence cardiovascular morbidity. We tested the association of lower airway caliber, obstructive sleep apnea (OSA), and other asthma-related factors, with systemic hypertension (HTN). METHODS: Asthma individuals at specialty clinics completed the Sleep Apnea scale of the Sleep Disorders Questionnaire (SA-SDQ). Medical records were reviewed for diagnosed HTN, OSA and comorbidities, spirometry, and current medications. FEV1% predicted was categorized as ≥ 80 (reference), 70-79, 60-69, and < 60. SA-SDQ ≥ 36 for men and ≥ 32 for women defined high OSA risk. RESULTS: Among 812 asthmatics (mean age ± standard deviation: 46 ± 14 years), HTN was diagnosed in 191 (24%), OSA in 65 (8%), and OSA or high OSA risk (combined OSA variable) in 239 (29%). HTN was more prevalent in lower FEV1% categories (p < 0.0001), in subjects with OSA, and those with combined OSA variable (55 vs. 21% and 46 vs. 14%, respectively, both p < 0.0001). With adjustment for covariates, associations with HTN remained significant for some FEV1% categories (70-79% odds ratio = 1.60 [95% CI 0.90-2.87]; 60-69% 2.73 [1.28-5.79]; < 60% 0.96 [0.43-2.14]), and for OSA (2.20 [1.16-4.19]). The combined OSA variable in comparison with OSA alone demonstrated a stronger association with HTN (3.17 [1.99-5.04]) in a reiteration of this model. Inhaled corticosteroids (ICS) at lowest doses, in comparison to no ICS use had an independent ‘protective’ association with HTN (0.44 [0.22-0.90]). CONCLUSIONS: In this young population, worse lower airways obstruction and OSA were associated with HTN. In contrast, lower ICS doses attenuated likelihood for HTN. Adequate control of airway inflammation at appropriate ICS doses, and screening for OSA may reduce the burden of HTN in asthma.