Rationale for targeted rather than population based screening with C-reactive protein using the National Health and Nutrition Examination Survey (1999 to 2002)
Abstract
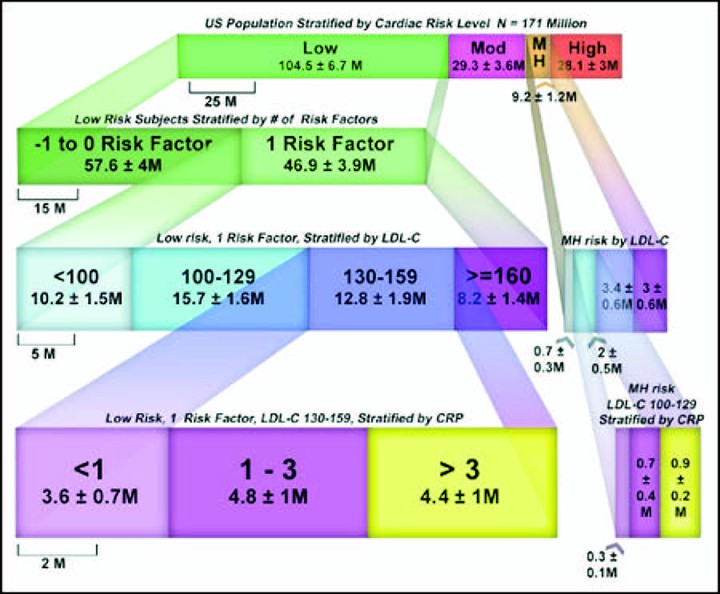
C-reactive protein (CRP) is the most well-studied inflammatory marker for the prediction of coronary artery disease. It was hypothesized that population-wide screening would have minimal impact but that a target population might be identified for whom CRP testing could be appropriate. The National Health and Nutrition Examination Survey (NHANES; 1999 to 2002) included 7,399 subjects who represented 171 million United States residents aged 20 to 79 years. Subjects were risk stratified according to National Cholesterol Education Program Adult Treatment Panel III guidelines. Subjects with CRP levels >3 mg/L then had their risk profiles adjusted by adding 1 risk factor and multiplying their Framingham risk scores by 1.5. Subjects had their low-density lipoprotein (LDL) cholesterol goals adjusted as necessary and were then recategorized as above or below their CRP-adjusted LDL cholesterol goal. LDL cholesterol goals were met initially by 67.8% (116 +/- 8 million) of United States residents, and 64.8% (111 +/- 8 million) achieved their LDL cholesterol goals after CRP adjustment. Thus, 5.3 +/- 1.1 million of the population (3.1 +/- 0.1%) had their risk modified in a clinically meaningful way by CRP adjustment. Targeting the screening to 2 groups, those with 1 risk factor and LDL cholesterol levels 130 to 159 mg/dl and those with moderately high risk and LDL cholesterol levels 100 to 129 mg/dl, we were able to identify all 5.3 million by screening only 14.8 million, achieving a screening yield of 35%. In conclusion, population-based screening with CRP provided a clinical impact for only 3.1% of United States residents. Patients with 1 risk factor and LDL cholesterol levels of 130 to 159 mg/dl and those with moderately high risk and LDL cholesterol levels of 100 to 129 mg/dl represent high-yield subgroups for routine CRP screening.