Abstract
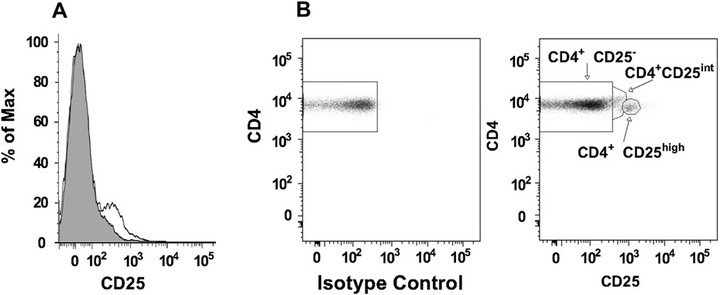
BACKGROUND: There is evidence that CD4(+)CD25(high) T-regulatory cells are important for establishing tolerance to allergens, but information in children is limited. OBJECTIVE: To test the hypothesis that greater numbers and function of CD4(+)CD25(high) T cells are associated with a reduced risk of childhood allergies and wheezing. METHODS: A cohort of 151 six-year-old children from atopic families was analyzed for peripheral blood CD4(+)CD25(high) and CD4(+)CD25(int) T cells by flow cytometry and for clinical and immunologic correlates of atopy. The associations between these variables were assessed by regression analysis. RESULTS: Factors positively associated with % CD4(+)CD25(high)/CD4 T cells were male sex, number of positive allergen-specific IgE tests, total IgE, season, and 1-month average total pollen count preceding blood draw. The percentage of CD4(+)CD25(high)/total CD4 T cells did not correlate with induced cytokine production, and correlated negatively with suppressive capacity of CD4(+)CD25(+) T cells (r = -0.45; P = .034). The percentage of CD4(+)CD25(int)/CD4 T cells was 54% higher in pollen-sensitized children compared with nonsensitized children in spring (P = .023 for interaction), and correlated positively with IL-5, IL-10, and IL-13 (P < or = .001 for all). CONCLUSION: Our findings suggest that blood CD4(+)CD25(high) cells are a mixture of activated and regulatory T cells, and that these cells could be seasonally regulated by environmental factors such as pollen exposure. CLINICAL IMPLICATIONS: Seasonal increases in CD4CD25(high) expression in children with allergy may represent systemic immune activation caused by pollen exposures.