The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXIII: the twenty-five-year incidence of macular edema in persons with type 1 diabetes
Abstract
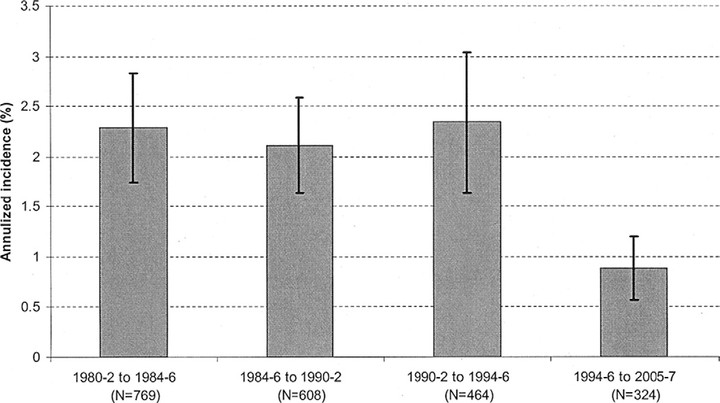
OBJECTIVE: To examine the 25-year cumulative incidence of macular edema (ME) and its relation to various risk factors. DESIGN: Population-based study. PARTICIPANTS: A total of 955 insulin-taking persons living in an 11-county area in southern Wisconsin with type 1 diabetes diagnosed before age 30 years who participated in baseline examinations (1980-1982) and at least 1 of 4 follow-up (4-, 10-, 14-, and 25-year) examinations (n=891) or died before the first follow-up examination (n=64). METHODS: Stereoscopic color fundus photographs were graded using the modified Airlie House classification and the Early Treatment Diabetic Retinopathy Study retinopathy severity scheme. Competing risk of death was included in statistical models. MAIN OUTCOME MEASURES: Incidence of ME and clinically significant ME (CSME). RESULTS: The 25-year cumulative incidence was 29% for ME and 17% for CSME. Annualized incidences of ME were 2.3%, 2.1%, 2.3%, and 0.9% in the first, second, third, and fourth follow-up periods of the study, respectively. In univariate analyses, the incidence of ME was associated with male sex, more severe diabetic retinopathy, higher glycosylated hemoglobin, proteinuria, higher systolic and diastolic blood pressure, and more pack-years of smoking. Multivariate analyses showed that the incidence of ME was related to higher baseline glycosylated hemoglobin (hazard ratio [HR] per 1% 1.17; 95% confidence interval [CI], 1.10-1.25; P<0.001) and higher systolic blood pressure (HR per 10 mmHg 1.15; 95% CI, 1.04-1.26; P=0.004) and marginally to proteinuria (HR 1.43; 95% CI, 0.99-2.08; P=0.06). CONCLUSIONS: These data show that relatively high 25-year cumulative rates of incidence of ME were related to glycemia and blood pressure. The lower risk of incident ME in the last period of the study may reflect recent improvement in care.