Changes in visual impairment prevalence by period of diagnosis of diabetes: the Wisconsin Epidemiologic Study of Diabetic Retinopathy
Abstract
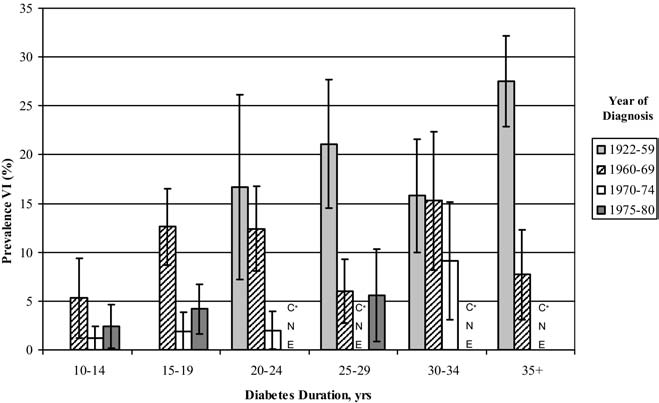
OBJECTIVE: To examine relationships of period of diagnosis of type 1 diabetes mellitus (T1DM) to the prevalence of visual impairment (VI). DESIGN: Population-based longitudinal study. PARTICIPANTS: Nine hundred fifty-five persons (3719 participant visits) 4 to 80 years of age at baseline who lived in an 11-county area in southern Wisconsin who were diagnosed with T1DM before 30 years of age contributed to the prevalence of VI. METHODS: Five eye examination visits occurred in the following periods: 1980 through 1982, 1984 through 1986, 1990 through 1992, 1995 through 1996, and 2005 through 2007. Age of diagnosis of T1DM was grouped as before 1960, 1960 through 1969, 1970 through 1974, and 1975 through 1979. Best-corrected visual acuity (VA) using a modification of the Early Treatment Diabetic Retinopathy protocol was measured. MAIN OUTCOME MEASURES: Visual impairment was defined as best-corrected VA in the better eye of 20/40 or worse. RESULTS: While controlling for duration of T1DM, there was a lower prevalence of VI for more recent periods of diagnosis of diabetes (odds ratio per category, 0.91; 95% confidence interval, 0.88-0.93; P<0.001). This remained while controlling for glycosylated hemoglobin, blood pressure, and other related factors. CONCLUSIONS: More recently diagnosed T1DM was associated with a lower prevalence of VI. This is likely because of the diminishing incidence of proliferative diabetic retinopathy (PDR) and clinically significant macular edema (CSME) resulting from better glycemic control and more timely interventions with photocoagulation for CSME and PDR in those with more recently diagnosed T1DM.