The 25-year incidence of visual impairment in type 1 diabetes mellitus the wisconsin epidemiologic study of diabetic retinopathy
Abstract
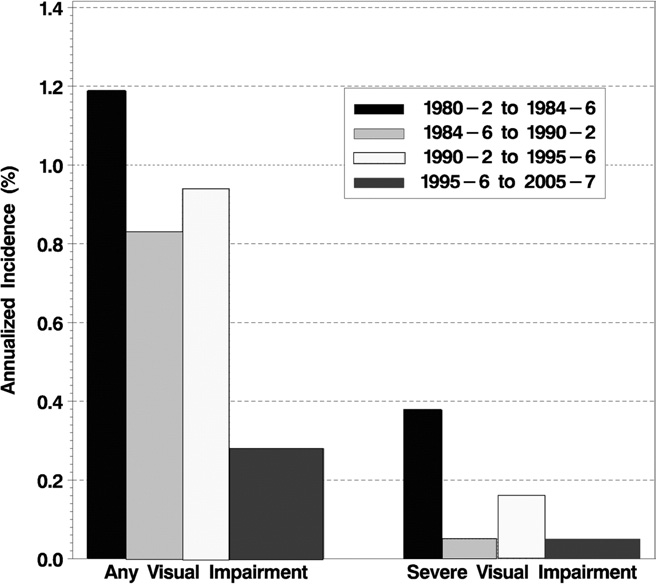
OBJECTIVE: To examine the 25-year cumulative incidence of visual impairment (VI) and its relation to various risk factors. DESIGN: Population-based study. PARTICIPANTS: Nine hundred fifty-five insulin-taking persons living in an 11-county area in southern Wisconsin with type 1 diabetes diagnosed before age 30 years who participated in a baseline (1980-1982) and at least 1 of 4 follow-up (4-, 10-, 14-, and 25-year) examinations or who died before the first follow-up examination (n = 64). METHODS: Best-corrected visual acuity (VA) was measured using a modification of the Early Treatment Diabetic Retinopathy Study protocol. Visual impairment and severe VI were defined as best-corrected VA in the better eye of 20/40 or worse and 20/200 or worse, respectively. MAIN OUTCOME MEASURES: Incidence of VI. RESULTS: The 25-year cumulative incidences of any VI and severe VI (accounting for competing risk of death) were 13% and 3%, respectively. Multivariate models showed increased risk of VI was associated (hazard ratio, 95% confidence interval, and P value) with more severe baseline retinopathy (1.14 per 1-step increase in retinopathy level; 1.03-1.27; P = 0.01), presence of cataract (2.49 versus absence; 1.53-4.04; P<0.001), higher glycosylated hemoglobin (1.28 per 1%; 1.16-1.42; P<0.001), presence of hypertension (1.72 versus absence; 1.05-2.83; P = 0.03), and currently smoking (vs. never smoked, 1.63; 1.01-2.61; P = 0.04), but not proteinuria. CONCLUSIONS: These data show that the 25-year cumulative incidence of VI is related to modifiable risk factors and, therefore, that VI may be reduced by better glycemic and blood pressure control and avoidance of smoking.