Abstract
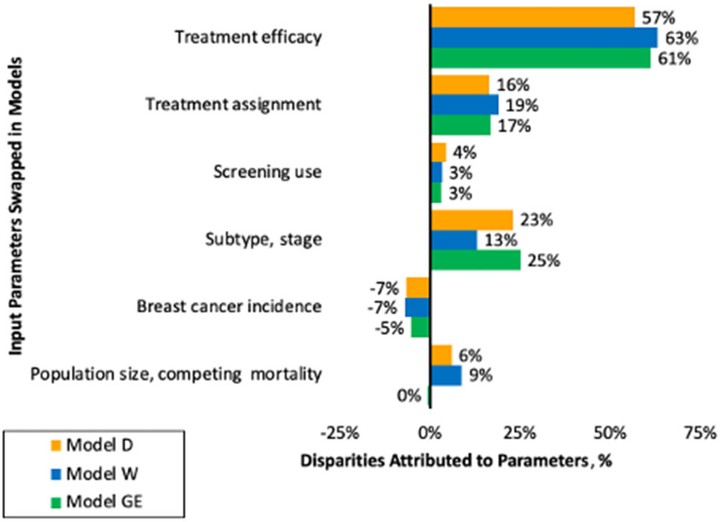
Background: Self-identified African American or Black women (“Black women”) have persistently higher breast cancer mortality than women from other self-reported racial/ethnic groups. These mortality differences are partially explained by the effects of systemic racism on cancer risk and carecontrol processes. We quantify the relative contributions of tumor factors, screening and treatment these cancer control processes on cancer mortality disparities. Methods: We used three Cancer Intervention and Surveillance Modeling Network (CISNET) simulation models to estimate the separate contribution of demographics, incidence, subtype, screening and treatment inequity on modeled mortality among multiple birth cohorts of Black women. Model input parameters were based on national data from registries and clinical trials. Results are summarized as the mean and range across the three models. Results: Results were very similar across the three models. Racial differences in tumor subtype and stage distributions in the absence of screening accounted for a median of 23% (range across models 13-24%) and screening accounted for a median of 3% (range 3-4%) of the modeled mortality in Black women. Treatment parameters accounted for the majority of modeled mortality for Black women: median 17% (range 16-19%) for treatment initiation and median 61% (range 57-63%) for real-world effectiveness. Conclusion: Our model results suggest that policies that decrease the effects of systemic racism on treatment access could increase breast cancer equity. The findings also highlight that improvements must extend beyond policies targeting equity in treatment initiation to include high-quality treatment completion. Future modeling research will be useful to test the effects of different specific policy changes on mortality disparities.