Abstract
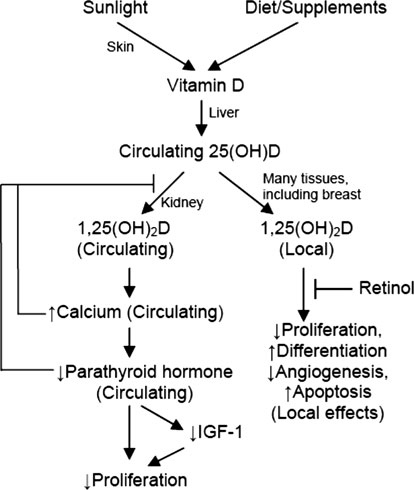
Laboratory studies have demonstrated that vitamin D has a number of chemopreventive properties, and that these properties may be mediated or modified by other molecules in the vitamin D pathway, such as parathyroid hormone (PTH) or calcium. However, there is little epidemiologic data exploring the effects of vitamin D on breast cancer risk in the context of these other molecules. We examined a panel of molecules in the vitamin D pathway in relation to mammographic breast density, a marker of breast cancer risk, in the Wisconsin Breast Density Study. A total of 238 postmenopausal women (ages 55-70, with no history of postmenopausal hormone use) were enrolled from mammography clinics in Madison, Wisconsin. Subjects provided blood samples that were analyzed for levels of 25-hydroxy vitamin D [25(OH)D], PTH, insulin-like growth factor-1 (IGF-1), IGF-binding protein 3 (IGFBP-3), retinol, and calcium. Percent breast density was measured using Cumulus software. In age-adjusted analyses there was a positive association between 25(OH)D and percent breast density (P = 0.05; mean percent density = 11.3% vs. 15.6% for 1st vs. 4th quartile of 25(OH)D). Breast density was inversely associated with PTH (P = 0.05; 16.0% vs. 11.4% for Q1 vs. Q4) and positively associated with the IGF-1:IGFBP-3 molar ratio (P = 0.02; 11.9% vs. 15.6% for Q1 vs. Q4). However, these associations were all null after further adjustment for body mass index (BMI; P > 0.25). The independent relation between 25(OH)D and breast density remained null among subgroups defined by BMI and serum levels of retinol, calcium, and estradiol. These results suggest no strong independent associations between the circulating molecules of the vitamin D pathway and mammographic breast density in postmenopausal women. While it remains possible that vitamin D could influence breast cancer risk, our results suggest that such an effect would be mediated through pathways other than breast density.